 |
Retinoblastoma |
Childhood Cancer Name:
Retinoblastoma
Explanation:
Retinoblastoma is a type of cancer that starts in the nerve cells lining the back of the eyeball (retina), although rare, retinoblastoma is the most common eye tumor in children.
The eyes develop in the womb, the eyes have cells called retinoblasts that divide into new cells and fill the retina. At a certain point, these cells stop dividing and develop into mature retinal cells. The retina is the structure at the back of the eye that senses light. It sends images to the brain, which interprets them, allowing us to see. Rarely, something goes wrong with this process. Instead of maturing into special cells that detect light, some retinoblasts continue to divide and grow out of control, forming cancer known as retinoblastoma.
Characteristics:
It is the most common eye tumor in children and it usually occurs before the age of five. It can occur in one eye (unilateral) or in both eyes (bilateral). If left untreated, retinoblastoma usually grows, making the eye blind and painful. IT MAY ALSO SPREAD BEYOND THE EYEBALL.
Biology:
The tumor develops when there is a gene abnormality on chromosome number 13. Genes are the instructions in the cell and they tell the cells how to grow.
The normal RB1 gene helps keep cells from growing out of control, when there is a mutation in this gene, people have a mistake in the instructions in their cells, and the cells keep growing without control.
This abnormal gene may be inherited either from a parent or happen for the first time at an early stage of development in the womb.
90% of retinoblastoma cases develop “out of the blue” and without warning.
10% have a family member with retinoblastoma.
In the developed world, and if diagnosed in an early stage retinoblastoma can be cured successfully using a range of treatments and 98% of children will survive retinoblastoma.
Main types:
- Congenital (hereditary) retinoblastoma
- Sporadic (non-hereditary) retinoblastoma
- Intraocular retinoblastoma (within the eye)
- extraocular retinoblastoma (cancer has spread beyond the eye)
Special cases:
- Trilateral retinoblastoma: Refers to a syndrome that occurs in 5% to 15% of patients with heritable retinoblastoma defined by the concurrence of bilateral retinoblastoma and a pinealoma (tumor in the pineal gland, a small endocrine gland in the brain).
- Progressive retinoblastoma: is retinoblastoma that does not respond to treatment. Instead, cancer grows, spreads, or gets worse.
- Recurrent retinoblastoma: is cancer that has recurred (come back) after it has been treated.
- Congenital (hereditary) retinoblastoma: About 1 out of 3 children with retinoblastoma have a germline mutation in one RB1 gene meaning all the cells in the body have a defective RB1 gene. For most children (75%) this mutation happens sporadically during the development inside the womb. The other (25%) of children have inherited it from one of their parents. Kids who carry the genetic mutation usually get more than one tumor and are likely to develop the disease in both eyes. Most children with hereditary retinoblastoma do not have an affected parent. However, these children can still pass their RB1 gene mutation on to their children.
- Sporadic (non- hereditary) retinoblastoma: 2 out of 3 children with retinoblastoma do not have the RB1 gene mutation in all the cells of their body. Instead, the RB1 mutation happens early in life and first occurs only in one cell in one eye, it’s not clear what causes these changes.
The stages of Retinoblastoma are:
- For treatment purposes, Staging categorizes retinoblastoma that is either intraocular (is found in one or both eyes but does not extend beyond the eye) or extraocular (cancer has spread beyond the eye to tissues around the eye or to other parts of the body).
- Several intraocular staging systems have been in use for many years to help doctors plan treatment. However, the recent success of clinical trials (research studies) demonstrating the effectiveness of chemotherapy to shrink tumors has led to the development of a newer staging system called the International Classification System.
For more information about the stages click here.
Childhood Cancer Localization:
Retina, eye.
Childhood Cancer Noticeable Symptoms:
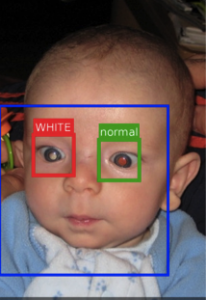
- A white color in the center circle of the eye (pupil) when the light is shone in the eye, such as when taking a flash photograph, eyes that appear to be looking in different directions, visual loss.
Parents often first detect it, because the parent notices white-eye in pictures of their children. This is why a Father of a Retinoblastoma patient created an app called “white eye detector” to help parents detect eye cancer in children.
Read more about it here.
- Patients with heritable disease present at a younger age, usually by 12 months.
- Most cases present with leukocoria also known as “Cat’s eye”, white-eye or glow. A child with a white pupillary reflex noted by the parents, identified in photographs or found on examination. Normally, the center of the eye appears red in response to the camera flash, but in retinoblastoma, the center of the eye may have a white glow.
- Strabismus is the second most common presenting sign, development of misaligned eyes over weeks to months.
- Vision problems: Some children are diagnosed as young babies because they do not appear to be developing normal vision. This can be detected with an electroretinography to measure vision (in small children) by measuring the electrical activity of the retina.
- Pain from increased pressure in the eye as the tumor grows.
- As the tumor progresses, patients may present with orbital or metastatic disease (in other parts of the body).
Childhood Cancer Diagnostic method:
Ophthalmic exam, ultrasound, magnetic resonance imaging (MRI).
- The heritable form of retinoblastoma tends to develop earlier in life (at age 12 months or less) than the non-inherited type (more commonly diagnosed at age 24-30 months).
- The diagnosis of retinoblastoma is usually made without pathologic confirmation. An examination by a pediatric ophthalmologist, usually under anesthesia. Some very young and older patients can be examined without general anesthesia.
Laboratory test:
- When a retinoblastoma is diagnosed, your child may have tests to check the exact position and size of the tumor.
- Blood test
- Ultrasound scan to determine thickness or height.
- Magnetic resonance imaging (MRI) scan, used to evaluate intra / extraocular and intracranial extension.
- Tumor staging (i.e. bone marrow examination, lumbar puncture and/or radionuclide bone scan) should be performed only in patients at risk of extra-ocular metastases.
Genetic Counseling:
Genetic counseling is an integral part of the management of patients with retinoblastoma and their families, regardless of clinical presentation.
- Blood and tumor samples can be tested to determine whether a patient with retinoblastoma has a mutation in the RB1 gene. Once the patient’s genetic mutation has been identified, other family members can be screened directly for the mutation with targeted sequencing.
- If there is more than one retinoblastoma, affecting one or both eyes and/or if any other relatives have had this disease, it is crucial to get genetic counseling and tests.
- The first step is, therefore, to find out whether any relative had retinoblastoma, then to examine if the parents as well as any brothers and sisters for retinal tumors or tumors in other parts of the body.
- Common practice for the parents and siblings of patients with retinoblastoma is to have screening ophthalmic examinations to exclude an unknown familial disease. Siblings continue to be screened until age 3 to 5 years or until it is confirmed that they do not have an RB1 gene mutation.
Parents tip:
If you recognize this sign in a photo, contact a doctor or the parents of the child immediately.
Childhood Cancer Treatment:
The type of treatment is individualized depending on a number of factors including number (one eye or both), the location of the tumor, size of the tumor, and visual prognosis.
- The main priority is to save the life; the next objective is to conserve as much vision as possible.
- It includes a multidisciplinary team of pediatric oncologist, ocular oncologist and pediatric ophthalmologists, radiation pediatric oncologist as well as other specialists.
- If the ophthalmologist feels that useful vision cannot be obtained, then removal of the eye (enucleation) is recommended.
- The standard for the treatment of retinoblastoma has been evolving and newer approaches have increasingly avoided radiation therapy, when possible. These newer approaches often involve the use of chemotherapy.
- If the tumor is too large for ‘focal’ therapy (i.e. laser photocoagulation, cryotherapy) can first be treated with chemotherapy to reduce tumor size until is small enough for laser or cryotherapy.
Types of treatment:
- Laser therapy: a laser is used to destroy blood vessels that supply oxygen and nutrients to the tumor.
- Cold treatment, cryotherapy: uses extreme cold to kill cancer cells.
- Heat treatments: This process uses heat to destroy the cancer cells and may be combined with chemotherapy or radiotherapy.
- Chemotherapy: chemotherapy may help shrink a tumor so that another treatment may be used to remove the remaining cells. In these cases, Chemo may also be injected around the eye (periocular) for local treatment.
- Stem cell transplant: to replace blood-forming cells in the bone marrow that have been killed by chemo and/or radiation.
- Local Chemotherapy:
- Intra-arterial chemotherapy: It is not commonly used and tends to be reserved for tumors that have not responded well to the standard treatment or if a tumor comes back. The procedure involves passing a tiny catheter (plastic tube) through the femoral artery (the artery in the groin), all the way up until it is in the ophthalmic artery (the artery in the eye).
- Intra-vitreal chemotherapy: Children who have developed seeds (small leftovers of the tumor) in the vitreous (the jelly part of the eye) may be offered injections of chemotherapy directly into the eye.
- Radiation therapy: uses high-energy rays from a machine to destroy the cancer cells. Important structures and vulnerable tissues surround the eyes; it’s essential to treat cancer of the eye with radiation that can be carefully controlled.
- Plaque Radiotherapy: by placing a temporary radioactive implant known as a plaque behind the eye for a few days.
- External beam radiotherapy: A beam of radiation is directed at the tumor via an x-ray machine called a linear accelerator.
External beam radiation therapy has two modalities Intensity-modulated radiation therapy (IMRT) and Proton beam therapy (PBRT) Early results with proton beam therapy are promising, especially in patients who showed no response to other treatment modalities, but it’s still fairly new, and there is very little long-term data on its use for retinoblastoma.
Only about 15 centers do proton beam therapy in the United States at this time.
Many centers now use newer types of external radiation therapy, which can target the tumor more precisely. This lowers the doses that surrounding normal tissues get, which may help reduce side effects. https://www.floridaproton.org/cancers-treated/pediatric-cancer/retinoblastoma - Side effects: sometimes causes cataract, damage to the retina (the inner lining at the back of the eye), and the optic nerve if it was in the area being treated.
It is sometimes possible to reduce the radiation damage and hopefully improve or maintain sight by giving injections of drugs into the eye, such as bevacizumab (Avastin). - For more about the side effect of radiotherapy and how to cope with them click here.
- Surgery: to remove the eye, if needed.
- Enucleation: If the tumor is very large and has damaged the sight in the eye beyond repair, then the ophthalmologist will recommend that the eye removed. This operation is called an enucleation.
Enucleation is only recommended when it is felt other treatments would not be effective, and/or would put the child’s life at risk. When that one eye is removed, in cases, which only that one eye was affected, more than 90 percent of those patients do not need any additional treatment. In patients with both eyes affected: if one eye is removed, treatment will focus on saving the remaining eye.- Learn more about how families cope with enucleation, click here.
About treatment
- Most patients with retinoblastoma can be cured, especially if the disease is confined to the eyes. If untreated, it spreads within and outside the brain and is rapidly fatal.
- Retinoblastoma treatment is highly effective if the disease is caught early.
Late effects of the treatment:
- Diminished orbital growth: If the eye has to be removed the eye socket (orbit) on that side may not grow as much as the other, leading to asymmetry. This can be prevented by use of correctly sized eye implants.
- Visual-loss: Patients with retinoblastoma demonstrate a variety of long-term visual-field defects after treatment for their intraocular disease, local chemotherapy, laser or radiation. For example after whole eye radiotherapy children may develop a cataract (clouding of the lens of the eye).
- Hearing loss: Carboplatin is commonly used in chemotherapy for retinoblastoma and this medicine can cause long-term hearing loss.
- Very young children who are diagnosed with retinoblastoma in one eye can develop a tumor in the second eye several weeks, or even months, later so regular eye examinations are very important.
- Patients with treated retinoblastoma as well as siblings who are at risk of inheriting the tumor need to be monitored indefinitely.
- Every 3-4 months until age 3-4 years, every 6 months until age 5-6, at about age 8 years can be examined annually. The patient and parents should be warned about signs of secondary tumors during these examinations so in any case they can call and visit the doctor. This may vary according to your doctor and treatment.
Experts:
Treatment requires a multidisciplinary highly specialized approach.
This tool can help you find a treatment Cancer Center specialized in Retinoblastoma near you: One Retinoblastoma World
Here are some of the top doctors in the field:
-
- For treatment modalities to save the eyes of children with retinoblastoma:
- Expert of pediatric intraocular tumor, Jonathan Kim. MD, Director of the Retinoblastoma Program at Children’s Hospital Los Angeles.
- Ophthalmic Oncologist, David H. Abramson, MD from Memorial Sloan Kettering Cancer Center
- For recurrent retinoblastoma: Ophthalmologist W. Harbour, M.D. from Bascom Palmer Eye Institute:
- For intra-arterial chemotherapy for retinoblastoma,Pierre Gobin, M.D, Interventional Neuroradiology, from Weill Cornell Medical Center:
- Retina and Vitreous Specialist Paul L Kaufman, MD from Thomas Eye Group.
- Ophthalmologist Brenda Gallie, MD from SickKids, Toronto, Ontario.
Testimonials Links:
Follow up:
- Very young children who are diagnosed with retinoblastoma in one eye can develop a tumor in the second eye several weeks, or even months, later so regular eye examinations are very important.
- Patients with treated retinoblastoma as well as siblings who are at risk of inheriting the tumor need to be monitored indefinitely.
- Every 3-4 months until the age of 3-4 years, every 6 months until the age of 5-6, at about the age of 8 years can be examined annually.
The patient and parents should be warned about signs of secondary tumors during these examinations so in any case they can call and visit the doctor. This may vary according to your doctor and treatment. - Periodic examinations of the unaffected eye are performed until the germline status of the RB1 gene is determined.
- Children with a germline Rb1 mutation may continue to develop new tumors for a few years after diagnosis and treatment and they need ongoing surveillance. Commonly examination is repeated every 2-4 months for at least 28 months. Regular brain scans to detect any brain tumor as early as possible.
- Children with the non-heritable type of retinoblastoma – which is the most common type – are not thought to be at any greater risk of secondary cancers than anyone else.
- Regular sight tests to ensure that they can see.
- Regular hearing tests in case any of the therapeutic agents have impaired hearing.
The main goals include:
- Preserve patient´s life.
- Preserve as much vision as possible.
- Decrease risk of late sequelae from treatment, particularly subsequent neoplasms (SNs).
Links for more information:
- Gov–General and medical information.
- The Children’s Oncology Group (COG), a National Cancer Institute-supported clinical trials group, is the world’s largest organization devoted exclusively to childhood and adolescent cancer research.
Here you can find follow-up recommendations for kidney health according to the chemotherapy of choice: https://childrensoncologygroup.org/index.php/organs/kidneyhealth - Fighting retinoblastoma resources (really useful links for parents about a lot of different subjects related to retinoblastoma)
- Retinoblastoma survivors network:
- Retinoblastoma detailed guide, American Cancer Society:
- A Parent’s Guide to Understanding Retinoblastoma:
- The Retinoblastoma (Cancer) Online Support Group:
- Patient trusted medical information and support:
- Cure search: A blog about children’s cancer survivors, fighters and supporters:
- Eye Cancer Heroes:
- Children Diagnosed With Cancer: Understanding the Health Care System (also available in Spanish) https://www.cancer.org/treatment/children-and-cancer/when-your-child-has-cancer/during-treatment.html
- Childhood cancer survivors face unique risks as adults:
Research:
Hospitals & Treatment Centers:
- St. Jude is the only pediatric cancer research center that does not charge its patients´ families for treatment that is not covered by insurance. Thus, St. Jude has never refused to treat a child because of the family’s inability to pay.
Learn more here. - St. Judes: https://www.stjude.org/disease/retinoblastoma.html
- Mayo Clinic: http://www.mayoclinic.org/diseases-conditions/retinoblastoma/symptoms-causes/dxc-20156215
- https://medlineplus.gov/genetics/condition/retinoblastoma/
- American Cancer Society: http://www.cancer.org/cancer/retinoblastoma/detailedguide/retinoblastoma-what-is-retinoblastoma
- Pediatric Oncology Resource Center: http://www.ped-onc.org/
- https://www.mskcc.org
- The American Society of Clinical Oncology: http://www.cancer.net/cancer-types/retinoblastoma-childhood
- National Cancer Institute: https://www.cancer.gov/types/retinoblastoma
- Cancer Research UK: http://www.cancerresearchuk.org/about-cancer/cancers-in-general/cancer-questions/eye-cancer
- Kids health: http://kidshealth.org/en/parents/retinoblastoma.html#
- University of California San Francisco, Ocular Oncology Services: http://www.itumor.org/retinoblastoma-spare.html
- Yale Cancer Center: http://www.medicine.yale.edu/cancer/patient/programs/pediatric/info/info.aspx?id=CDR62846
- Childhood Cancer Name:
- Explanation:
- Characteristics:
- Biology:
- Main types:
- Special cases:
- Childhood Cancer Localization:
- Childhood Cancer Noticeable Symptoms:
- Childhood Cancer Diagnostic method:
- Laboratory test:
- Genetic Counseling:
- Parents tip:
- Childhood Cancer Treatment:
- Late effects of the treatment:
- Experts:
- Testimonials Links:
- Follow up:
- Links for more information:
- Research:
- Hospitals & Treatment Centers: